OPIOID ADDICTION
It is very important to remind ourselves of the motivating factors present for change. Opioid addiction is an ‘ambivalent disease.’ This means that most people who struggle with this condition experience internal conflict. There are countless reasons why you need to change and strangely multiple reasons to keep the addiction going. Examples of reasons to change include medical problems, legal issues, or simply feeling like a slave to opioids. Reasons to stay the same are feeling ashamed about your addiction, potential conflicts in a peer group, or simply a sense that change is just too hard!
To start this session, try and list 3 primary reasons to keep things the same and 3 reasons to stop using opioids:
- 3 Reasons to Continue Using Opioids
- 3 Reasons to Stop Using Opioids
This session will focus on some early recovery topics that you need to be aware of:
- Overdose education and prevention
- Basic medical screening for Hepatitis C, HIV, or common health conditions
- MAT education in early stabilization phase
- Pitfalls to staying in treatment
Overdose Education and Prevention
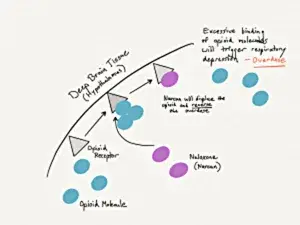
Opioid addiction can be quite lethal and a common cause of death is from an overdose. The cause of death is actually due to your breathing center shutting down and the brain not getting enough oxygen. If you have experienced an opioid overdose before, talk to your provider about this. People who have been going through a transition in their opioid use are the highest risk group for experiencing an opioid overdose. This includes you at this time. Treatment disrupts the status quo and, through that disruption, moves you towards a position of health or worsened disease.
A good recommendation at this phase to help provide some extra safety is to obtain a naloxone kit. Naloxone is the antidote to an opioid overdose. It comes in a few different forms such as a muscular injection in your shoulder or an intra-nasal spray. Most pharmacies stock naloxone medication, as this is now legal to be in the hands of the public in almost all US states. It used to be available only for emergency medical providers. It’s important to remember that someone witnessing the overdose victim will likely need to administer this medication. This emergency approach is ideal for people living with a family who understand the struggle with opioid addiction and are aware that you are changing.
Receiving a naloxone dose is not harmful to the body, but it will feel quite miserable. This medication instantly removes the heroin or opioid painkiller from your brain, placing you into opioid withdrawal. Most importantly, though, you’re alive. The news talks about the opioid epidemic constantly and may be one of the reasons you sought treatment to change your life. We start this whole process and your arc of recovery by emphasizing safety above all else.
Additional Medical Needs
It is very common for those struggling with opioid addiction to start using needles for IV drug use, and with this comes the risk for Hepatitis C and HIV infection. As you are starting out with your recovery arc, your provider should be able to address some of these issues with you and offer testing to see if you have contracted one of these infections.
Although these are scary, both Hepatitis C and HIV are well-treated conditions these days. As compared to the 1980’s and 1990’s, most people are no longer dying from HIV. It’s a chronic, manageable disease rather than a death-sentence, provided you stick with your provider’s treatment recommendations and take necessary medication. If HIV goes untreated, it will progress to AIDS and eventual death.
Sexual health issues also are good to address in early recovery. This includes testing for sexually transmitted diseases (and pregnancy if you’re a woman). Talk to your provider and get information about birth control options and safe sex practices.
In addition to the infectious diseases, many people who enter recovery from opioid addiction discover that they have another common baseline health problem such as high blood pressure. As you are starting to address your health and stability, please work with your provider to build the necessary treatment plans to manage anything that might be going on in your body. Recovery is all about health!
MAT Education
Buprenorphine is a partial opioid, methadone is a full opioid, and naltrexone is an opioid antagonist (blocker). This means that these medications function very differently in the brain. If you are using an MAT approach at this stage in your recovery, you will need to be aware of the basic chemistry that’s taking place.
Let’s review each of these medications briefly.
Buprenorphine
Overall, buprenorphine really shines as a medication approach in three primary zones:
- Alleviating opioid withdrawal
- Preventing addictive opioid use “over-the-top” of the buprenorphine
- Craving reduction
The buprenorphine molecule in the brain actually binds much more tightly than typical opioids. This is positive in that it provides some drug-use protection if you were to use pills or heroin, but has some issues during the ‘induction phase’ of your care. Because it binds so strongly, it will essentially kick off existing opioids in the system and may cause the phenomenon of precipitated withdrawal. This is rarely dangerous, but can be uncomfortable for a brief period. If this happens, and you feel like something is significantly wrong, talk to your doctor or seek urgent care. Probably the biggest risks are for those who have heart disease, high blood pressure, or fluid-balance problems and dehydration (the precipitated withdrawal can cause diarrhea and fluid losses).
Once you settle into a maintenance dose, heroin will have a hard time kicking out the buprenorphine. People given this medication for their opioid addiction have statistically significant reductions in opioid use and death. They also have greater treatment retention.
Methadone
This medication is a full agonist. That means that there is an overdose potential from taking this medication and that potential cannot be ignored because methadone overdoses are often quite lethal. Methadone cannot be prescribed by standard physicians or in an office setting. It must be dispensed through a structured methadone clinic. Advantages of this medication actually are connected to all the services you are provided through a daily monitoring clinic and the associated accountability.
Problems with methadone include some potential issues with electrical conduction in your heart (your medical team will test for this) and issues of combination with other substances. It is also possible to use heroin or painkillers in addition to methadone, unlike with Buprenorphine and its blockade effect. Additional problems with methadone involve the exposure to other active drug users in the clinic environment and risks for being offered drugs of different sorts while trying to get clean. If you experience anything like this, contact your center or doctor immediately. Your treatment environment should be of the utmost safety and support for you.
Naltrexone / Injectable Naltrexone
Unlike Buprenorphine or Methadone treatments (which are called Opioid Replacement Therapy or ORT), naltrexone is an abstinence treatment and blockade approach. Naltrexone blocks opioids from acting in the brain and prevents them from getting you high, overdosing, or giving pain relief. This approach leads to behavioral extinction – if you aren’t getting any effect from the pills or heroin you buy, eventually you’ll stop wasting your money.
A naltrexone injection, called Vivitrol, will last for 30 days. This is very protective during your stabilization phase, but may not be enough total time to really change your life. Fortunately, the injections can happen back-to-back, and I have had multiple successful people receive 12 consecutive naltrexone injections.
The cost of Vivitrol out-of-pocket is quite high ($1100 per month). If you are pursuing this approach, there are good assistance programs such as “TouchPoints” available to you. This is a web service offered by the manufacturer of Vivitrol to decrease the cost by about 50%. Insurance also does reasonably well in covering this medication for opioid addiction.
Probably the biggest dilemma with using injectable naltrexone with people is that the person will need to detox from heroin or painkillers completely prior to receiving a Vivitrol shot. Bridging people onto Buprenorphine medication seems to be markedly easier. Some of the most successful cases moving onto injectable naltrexone seem to be those in residential treatment centers. Typically, the person goes through required detox from opioids in a safe environment and then a medication such as this is used to stabilize early recovery and drug usage.
Read more CeDAR Education Articles about Opiate Addiction including Moving from Painkillers to Heroin.
