ADDICTION SCIENCE
Sleep: Part 3 of 3
This is our third installment for articles regarding sleep and insomnia. We are going to review one of the most evidence-based approaches to treating insomnia through a therapy and behavioral intervention. This program is called Cognitive Behavioral Therapy for Insomnia, or CBT-I. This program has different parts including the topics of sleep hygiene, stimulus control, passive wakefulness and sleep logs. If you or a family member has struggled with insomnia and are seeking an alternative to meds (and a more lasting approach), CBT-I may be a perfect fit for you. It is important to acknowledge that CBT interventions are effective for a multitude of conditions. These include addiction to substances, major depression or different anxiety disorders. CBT tends to emphasize the triangle of thoughts, emotions, and behaviors. We help people build insight into their anxiety or moods through this approach. We also help people understand dysfunctional patterns with current sleep behaviors. 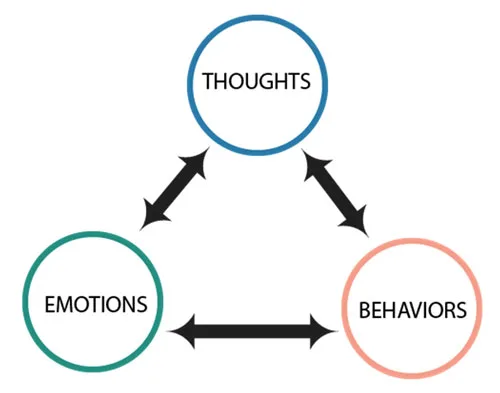 At CeDAR, we make a strong effort in promoting these interventions instead of being completely reliant on medication approaches. Those looking to recover from addiction need to be mindful of how substances had been their most-used coping skill over the years, hence they are likely prone to lean too heavily on pills. This is where CBT-I comes in.
At CeDAR, we make a strong effort in promoting these interventions instead of being completely reliant on medication approaches. Those looking to recover from addiction need to be mindful of how substances had been their most-used coping skill over the years, hence they are likely prone to lean too heavily on pills. This is where CBT-I comes in.
Sleep Hygiene
Our bedtime routine with all of its variables is called sleep hygiene. Just as with everyday hygiene, our goal with sleep hygiene is to be a good caretaker of ourselves. Some people practice effective and healthy sleep practices, while others do not. What things should you look for in reviewing your own sleep hygiene? These examples are practices to help yourself get in a good position to fall asleep:
- Pay a lot of attention to how your bedroom is arranged. Where does light come from? Are there ways to make the room exceedingly dark when you’re trying to fall asleep?
- Avoid clocks! Noticing the time each evening only makes you restless and can feed your insomnia. Look for a way to use the alarm feature of an electronic device or watch, or even turn your clock around when you’re sleeping so as to avoid the distraction.
- Have a dedicated sleep routine. This will involve typical things such as tooth brushing and pajamas. The routine is very helpful in settling down our minds and sticking with something familiar.
Stimulus Control
As CBT-I is all about an overall training program for your brain, it makes sense that it also includes daytime patterns. To achieve quality sleep, a person essentially needs to create a daytime of wakefulness in contrast to a nighttime of sleepiness. This also means that the person needs to gradually be winding down over the later parts of the day, so as not to build further neuro-stimulation and difficulty falling asleep. Examples for this topic include:
- Pay attention to caffeine intake, specifically trying to avoid it later in the day.
- Avoid alcohol or other substances approaching bedtime (this is a no-brainer for those working a recovery path from addiction).
- Take showers usually in the morning to promote wakefulness. Consider baths in the evening to promote winding down and peace.
- Exercise earlier in the day. The same principles for showers apply to exercise – you’re trying to pay attention to how you become more or less stimulated.
- Completely avoid naps! This is an absolute must for effective stimulus control. Sleeping during the day will disrupt the rhythm of what you are trying to do. While creating rest and briefly helping you feel better, it will soften your sleep drive during bedtime, leading to surface-level sleep. This, in turn, will make you more tired and craving a nap during the day. The cycle continues in this fashion.
Sleep Logs
As our goal with CBT-I is to help improve your quality of sleep, part of this involves conditioning yourself to be asleep during times you are in bed. This is in contrast to people who may be in bed for a few more hours than they are actually asleep, either deliberately or amidst their tossing and turning. Sleep logs shed some light on your patterns by tracking the total number of hours you are lying in bed and comparing this to your estimated hours of physically being asleep. This creates your “sleep ratio.” Healthy sleepers will often have a sleep ratio of around 90%. To determine your sleep ratio, it should be an average over at least the past week. Write down on a chart the time you fall asleep and the time you wake up. Try and make your wake-up time fixed and consistent each day with your alarm. This consistency helps you with overall sleep rhythm.1
Sleep Ratio
Sleep Ratio = Hours Sleeping / Hours Lying in Bed
For instance, if you lie down one night at 10:00 pm, fall asleep at 11:00 pm, and wake up at 6:00 am, you were physically asleep for 7 hours and in bed for 8 hours. Your sleep ratio would be 7/8. If you woke up for an hour stretch of time in the middle of the night, your sleep ratio would then be 6/8. Keep in mind that your sleep log is an estimate. If we revisit themes of sleep hygiene, it is important to avoid keeping a visible clock next to your bed as this only leads to obsessing. Simply give it your best guess. Once you have an average ratio, you would adjust your sleep schedule so as to reach a target ratio of around 90%. This means that if you wake up at 6:00 am, and typically sleep for 7 hours, your target bedtime should actually be close to 11:00 rather than 10:00. Once again, the goal with this entire program is to effectively train yourself to sleep well and consistently. It might sound strange to lie down later in the evening if you struggle with insomnia, but this is exactly what you may need to do. The restless time in bed doesn’t actually help you and may contribute to more worrying and nights of poor sleep.
Passive Wakefulness
Anxiety and worry can be very destructive to a good night’s sleep. The skill of passive wakefulness helps decrease some of these worries, emphasizing mindfulness approaches. This helps a person pay attention to the patterns within their body, specifically sleepiness and the window in which they could attempt to fall asleep. This involves taking a trusting approach and not really ‘trying’ to fall asleep, but rather understanding the natural state of sleep and how your body will fall asleep on its own. When someone is using passive wakefulness, they would approach sleep this way and also make efforts to let go of frustration around insomnia. This can include using other trained mindfulness exercises covered in other articles. This also involves avoiding the tossing and turning of being wide awake in bed. Instead, the person would actually get up and read or do something peaceful if they experience lying in bed for around 30 minutes or longer. The ruminations about sleep tend to hurt rather than help, hence passive wakefulness seeks to move away from such thought patterns.
Who Can Benefit from CBT-I?
While this program was developed to help those with insomnia, it offers sensible and practical advice for anyone in the areas of good sleep behaviors and choices. Many people struggle with different degrees of insomnia, including some people with only mild disruptions in sleep. Paying attention to your sleep patterns can be helpful if you have an addictive disorder, a mental health condition or no significant daily struggle. Better sleep quality translates to better life performance for all people. If you are interested in learning more about CBT-I, there are many available online resources and books about the curriculum. We offer some of the introduction to these approaches through our CeDAR lecture series. Feel free to contact us or our family program if you’d like to learn more. Read more CeDAR Education Articles about Addiction Science 1
